For many years, the menstrual cycle was mainly influenced by the moon and it lasted 28 days - but those days are gone. Today, more busy lifestyle means that the length of the menstrual cycle varies considerably. Especially the first phase of the menstrual cycle is sensitive to many external factors, such as: the type and intensity of lighting, long distance travelling connected with climate zones and temperature changes, quality of sleep, nutritional status, fitness, exposure to chronic stress or variety of diseases.
The calendar method described by Ogino and Knaus no longer applies and it becomes more and more important for each woman to listen to the rhythm of her own body, being aware of the cyclical changes and to observe these changes regularly.
The following section of this article will discuss in detail some issues concerning the basic symptoms of fertility:
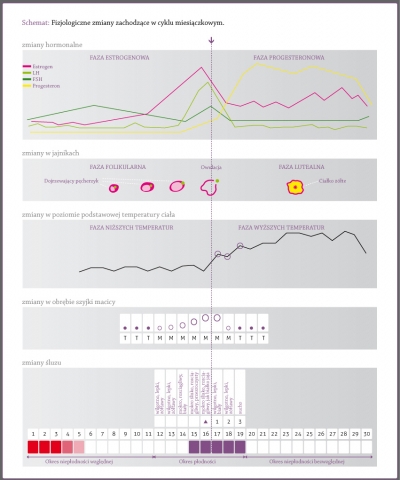
- The typical menstrual cycle is biphasic: menstruation begins, followed by the first preovulatory (estrogen) phase, and then there is the second - postovulatory (progesterone) phase.
- Nowadays the cycles lasting from 23 to 35 days are considered typical whereas irregular ones are those with the difference in length of more than 10 days. This factor causes that determining fertile days based on a standard 28-day menstrual cycle often results in an unplanned pregnancy.
- Hormonal changes cause a number of symptoms including: changes in the quality of cervical mucus, basal body temperature changes, changes in the cervix. Daily observation of these symptoms can determine with precision when we are dealing with the infertile (relative and absolute) phase and when it is the fertile phase
- The ability to fertilize the released ovum during the ovulation lasts for up to 12 hours (in the case of multiple ovulation for up to 24 hours), but due to sperm viability, it is assumed that the fertile period begins 5-6 days before possible ovulation.
- During each menstrual cycle the hormones are responsible for both physiological changes within the female genital organs and changes of her mood, physical and intellectual condition, as well as changes in skin condition and appearance. Awareness of these changes and ability to recognize them every day help to deal with periodically occurring ailments.
The course of a typical menstrual cycle
Menstrual cycle begins on the day of menstrual bleeding and ends the last day before the next bleeding. A typical cycle is biphasic, i.e., we can distinguish two successive phases: pre-ovulatory and postovulatory, separated by an ovulation . Contrary to popular beliefs, that moment isn’t often in the middle of the cycle but is located approximately 14 days before an expected bleeding.
During the preovulatory phase (also known as estrogenic or follicular), shortly after the end of menstruation, in the uterus there is the process of sloughed mucosa reconstruction due to the activity of the dominant hormones of this phase - estrogens. Simultaneously, there is growth and maturation of ovarian follicles; one of them gets a dominant position and develops as a Graafian follicle, and, when it becomes mature, it breaks and releases an egg during ovulation. The released egg is picked up by the hyphae of the fallopian tubes and directed inside, thus it begins its journey toward the uterus. After about 12-24 hours the egg - if it hasn’t been fertilized - dies and is excreted.
Postovulatory phase (also called progesterone or luteal) is dominated by the activity of the other hormone - progesterone. It is produced by the corpus luteum developed from a ruptured Graafian follicle and it is responsible for the changes of secretory endometrium. When there is no fertilization and implantation of the fertilized ovum in the uterus, the corpus luteum disappears (progesterone level drops), resulting in mucosal ischemia and thus its peeling which means menstrual bleeding. This is the beginning of the next menstrual cycle.
Menstruation prepares the uterus for the next cycle, during which the lining builds up and transforms again to create conditions for the possible implantation of human embryo.
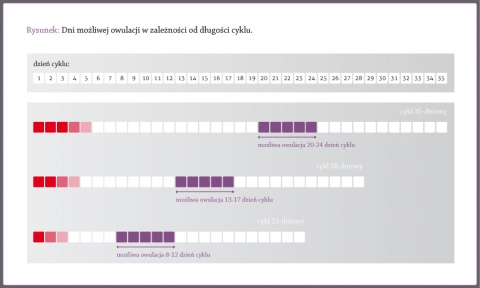
Currently the length of the menstrual cycle differs from the average 28-day cycle, and the cycles lasting from 23 to 35 days are considered typical. The irregular ones are those with the difference in length of more than 10 days. Differences of cycle lengths are observed mainly in the preovulatory phase, whereas the length of the postovulatory phase is quite regular and it is approximately 14 days. Consequently, identifying the fertile days from the date of the last menstrual period and calculate them based on a standard 28-day menstrual cycle might be incorrect and often ends with an unplanned conception. Only a comprehensive observation of the signals sent by female body allows to accurately determine the fertile days, so it is good idea to learn those signals and processes controlling them.
Hormonal changes associated with the particular phases of the menstrual cycle
The transformations occurring in the menstrual cycle are caused by hormonal changes. Hormones (chemicals) are secreted by the endocrine glands, on the basis of signals initiated by the brain and affect various body functions.
Every cycle includes two phases: preovulatory phase, dominated by the activity of estrogen and postovulatory phase when progesterone plays a major role. At the beginning of each cycle, after the start of menstrual bleeding, the hypothalamus stimulates the pituitary gland which begins to produce a hormone called follicle-stimulating hormone (FSH). This hormone stimulates the maturation process of growing follicles in the ovary. Maturing follicles also secrete hormones called estrogens which bring about renewing and growing of the endometrium, increase the secretion of cervical mucus, slight opening, raising and softening the cervix. High level of estrogens does not affect the basal body temperature, which remains at a relatively low level.
The concentration of estrogens reaches its peak about 24 hours before ovulation. At the same time there is a sudden burst of pituitary luteinizing hormone (LH). This hormone causes the rupture of a mature follicle, called now the Graafian follicle, and the release of the egg - ovulation. If for some reason there will be no burst of LH hormone or its concentration is too low, there is no ovulation, even if the follicle is matured.
After the ovulation, the estrogens level falls rapidly, reaching the minimum, then it rises slightly again and remains below the preovulatory level until the time of menstruation. The follicle, which released the egg, changing its character and becomes a corpus luteum secreting the hormone - progesterone. Higher level of progesterone is associated with a further thickening of the uterus lining and increase its blood supply, the inhibition of the next ovulation, the raise of basal body temperature by a minimum of 0.2 ˚ C, the mucus thickening and closing, lowering and hardening the cervix. These factors are a set of symptoms used to determine the beginning of the postovulatory infertility phase (absolute, certain).
The corpus luteum secretes progesterone for about two weeks. When there is no fertilization, its life is over, and level of progesterone decreases rapidly, which is accompanied by ischemia, and then peeling the uterus lining and its excretion in the form of menstrual bleeding. If the egg is fertilized, the pregnancy corpus luteum appears having a similar function to the menstrual corpus luteum, but for about 16 weeks. Then it gradually disappears.
How do you ovulate and how can you determine the moment of ovulation ?
In the ovaries there are follicles in various stages of development. Most of them are primary follicles, which each female child is provided with during her fetal life. The follicles number is decreasing gradually until they are used up during the premenopausal period.Due to FSH activity the primary follicles gradually transform into growing ones, several of them into the matured ones, and then one of them into the Graafian follicle, which releases the egg during an ovulation.
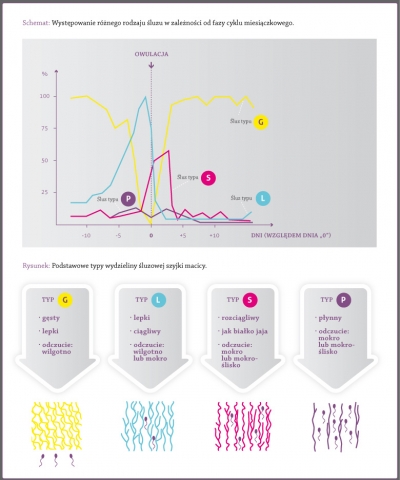
During the periovulatory period the secretion produced by the cervix has the most fertile features, namely it is very stretchy, it gives the feeling of wetness and slippery, it is clear, crystal and resembles egg white. After the peak day - the last day of fertile type of mucus, there is a significant lowering of its quality and fast disappearance.
Ovulation is a very complex process, which involves many chemicals with hormonal activity, and this process can be often disturbed. The exact moment of ovulation is difficult to identify precisely. Indicators which inform us about the forthcoming ovulation are: the level of Graafian follicle growth observed by ultrasound, increased LH level and also the change of cervical mucus characteristics. We can assume that ovulation has happened by: increased level of progesterone and a rise in basal body temperature, but it sometimes happens that, despite these symptoms, ovulation did not occurred (e.g. in case of luteinized unruptured follicle - LUF).
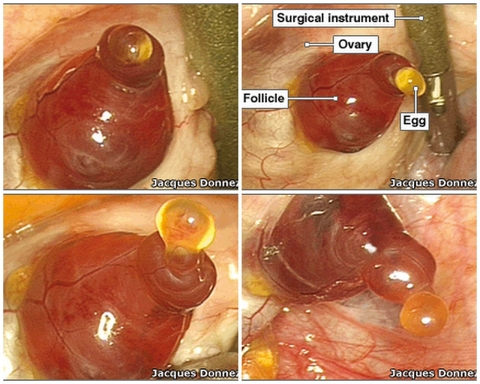
Using one of the natural fertility recognition methods developed by prof. J. Rötzer we can specify the moment of ovulation quite closely – it is based on observation of mucus and temperature measured after waking up and it falls on the peak day and the next day after it or on the day of the temperature drop just before its rise to the level of higher temperatures and in the first morning of temperature increase. The only evidence for the occurrence of ovulation is, however, to observe this phenomenon during the operation, as well as pregnancy.
The egg released during ovulation lives only for 12 hours (in the case of multiple ovulation up to 24 hours). The next ovulation in the same cycle is inhibited by the activity of progesterone secreted by the corpus luteum formed after bursting of the Graafian follicle. The moment of ovulation (it lasted 15 minutes) was recorded incidentally during hysterectomy:
Ovulation moment caught on camera.
During another surgery the moment of ovulation has been successfully recorded:
The figure below presents the possible ovulation days, depending on the length of the cycle - usually they are between 12th and 16th day before the next period.
How do the hormones dominant during the different cycle phases affect the cervix and the its mucus ?
Structure and function of mucus secreted in the crypts (glands on the sides) of the cervix and their connection with fertility were examined and described by prof. Erik Odeblad from the University of Umea in Sweden. He observed the presence of four types of cervical mucus: G, L, S and P.
The G-type mucus is thick, it closes the cervical canal during infertile days it is a barrier to sperm. It occurs usually just after the menstrual period, during the postovulatory phase and pregnancy. The P- type mucus produced in the highest cervical crypts causes dilution of the G – type one, giving the feeling of moisture in the vestibule of the vagina (the “W” feeling by the Rötzer’s method) and indicates the beginning of fertility phase. The L-type mucus occurs with increasing level of estrogens; it is sticky, stringy and opaque. With the high level of estrogens the mucus is getting clearer, stretchy, and gives the feeling of slipperiness, lubrication – this is the S –type mucus. In addition, due to estrogens, the cervix is getting softer and slightly opens, facilitating the penetration of sperm into the uterus and further to the fallopian tubes.
Periovulatory mucus contains both strands of S mucus (liquid gel) and lumps of L mucus (sticky gel), and the balance between them seems to be necessary to maintain the optimum level of fertility. According to prof. Odeblad the particles of L-type mucus are a frame for a smooth S- type mucus and they act like a filter for sperm which is probably not suitable for fertilization and facilitate transport of more efficient sperm. The mucus secretion of the close to ovulation period is composed of types S, L and the 4-8% of the P-type mucus, causing the intense slippery sensation thanks to dilution of the L and S-type mucus, which facilitates the transport of sperm into the uterine cavity. The presence of P-type mucus explains strong lubrication feeling without any visible signs of mucus on the outside (it is often the peak day).
After the ovulation, due to secreted progesterone, the cervix hardens and closes quite quickly creating so-called biological valve for the sperm. An additional barrier is thick and sticky G-type mucus. Professor Odeblad’s observations indicate the change of mucus secretion phase length with age. For 20- year – old women the average length of this phase is 4-5 days, whereas for 35-year-old women it lasts only 1-2 days. Similarly, the cervical mucus characteristics (its quality) change as well.
Based upon:
- E. Odeblad „The Discovery of different types of cervical mucus and the Billings Ovulation Method”, Bulletin Natural Family Planning Council of Victoria, 1994.
- E. Odeblad “Cervical Mucus and their functions”, Irish College Physicians and Surgeons, 1997.
See more: How to carry out the observations of fertility changes during the menstrual cycle?
What is the basal body temperature chart?
Looking at the basal body temperature chart, during the menstrual one can observe two phases: the lower temperatures and the higher temperatures phase. The lower temperatures phase begins in the early days of menstruation, but soon after ovulation the basal body temperature rises and remains higher until the next menstrual period.
The progesterone, produced by the corpus luteum formed after the bursting of the Graafian follicle, is responsible for the increase of basal body temperature after ovulation. The role of this hormone is to prepare the conditions for the implantation of the fertilized egg and the correct development of pregnancy. Menstrual corpus luteum function is continued for about 10 days, then it begins to disappear, causing the detachment of the top layer of the endometrium and its expulsion in the form of menstruation.
If the ovum is fertilized, the corpus luteum becomes pregnancy one. It produces large amounts of estrogens and progesterone which are necessary for the correct development of pregnancy. The increased progesterone production is maintained for about 16th week, until the task of pregnancy maintenance is taken over by developed placenta.
The main purpose of progesterone is to reduce the excitability of uterine contractions and prevent the premature expulsion of the fetus. The end of its secretion by the placenta in the final stage of pregnancy is usually a signal to start delivery.
See more: The detailed rules of determining infertile and fertile days.
When are your fertile and infertile days?
During the menstrual cycle there are three phases associated with changes in fertility:
The relative infertility phase. It begins with the menstruation and its end can be determined by a few basic principles based on the observation the temperature measured after waking up and the quality of cervical mucus. The length of this phase is not constant and it can vary in each cycle. For very short menstrual cycles the egg growing begins very early and in the last days of the menstruation the fertility phase starts (!). The Pearl index for this phase is less than 0.2%.
The fertility phase, lasts relatively short. A mature egg is expelled from a Graafian follicle (ovulation process) and travels through the fallopian tube, and its ability to be fertilized lasts up to 12 hours (in the case of multiple ovulation to 24 hours). Because of sperm viability for 5-6 days – such a period before the ovulation is assumed to be fertile one . The important, easy to observe symptoms of the fertility phase are: good quality mucus secreted by the cervix, the changes in the cervix and ovulation pain.
The postovulatory (absolute) infertility phase begins few days after ovulation from the disintegration of the egg and lasts until the next menstruation. The end of the fertile period is marked by increased basal body temperature of at least 0.2 ˚ C, observed for three consecutive measurements and lowering the quality of mucus secreted by the cervix and its quick disappearance. Pearl index for this phase is 0%, which means a certain infertility.
The influence of hormones on your mood and appearance
During the menstrual cycle the natural fluctuations of hormones in female body activate the reproductive processes which are reflected in changes within the genital area, external appearance and physical, emotional and intellectual ability.
The activity of estrogens during the first (preovulatory) phase of the cycle results in:
• maintaining a basal body temperature at an unchanged low level,
• the gradual regeneration of the endometrium,
• opening, lifting and softening of the cervix,
• changing the cervical mucus features from less fertile to more fertile.
In the period of the high estrogens level you can experience a very good mood, fitness improvement , greater efficiency and improved intellectual ability to concentrate, as well as increased libido and a more beautiful appearance. The estrogen phase is still unstable, is formed differently in each cycle and it is sensitive to stress, medication and other factors that may interfere with.
The effect of increased concentration of progesterone in the second (postovulatory) phase of the cycle causes:
• increase of the basal body temperature of at least 0.2 ˚ C,
• inhibition of the next ovulation,
• fuller breasts feeling
• changes in secretory endometrium (preparation for possible implantation of a human embryo),
• closing the mouth of the cervix, its lowering and hardening,
• thickening of cervical mucus.
During the progesterone phase you can often experience worse physical and emotional condition, the symptoms of fatigue and sleepiness, increased nervousness, a drop in concentration, intellectual ability lowering, decreased of libido and problems with skin.